The Evolution of Biomedical Research: From Petri Dishes to Organ-on-a-Chip Technology
Organ-on-a-chip (OOC) technology is a significantly used emerging technology in cell biology and biomaterials to replicate human organ functionality in laboratory settings. Also referred to as microfluidic devices, these help to mimic the specific organs by creating a natural environment for living cells and tissues. OOCs are transforming drug development and making it easier to understand human physiology and severe disease mechanisms; providing an ethical alternative that enables to get updated on traditional models.
OOCs are built using transparent materials such as polydimethylsiloxane (PDMS), enabling the observation of the real-time behaviour of cells. These devices have microchannels that are coated with human cells taken from the specific tissue, which can efficiently mimic the functionality of actual human organs and their specific activities, like lung expansion or heartbeats, by providing blood flow and applying mechanical forces similarly to the human body (1).
Multi- organ chip
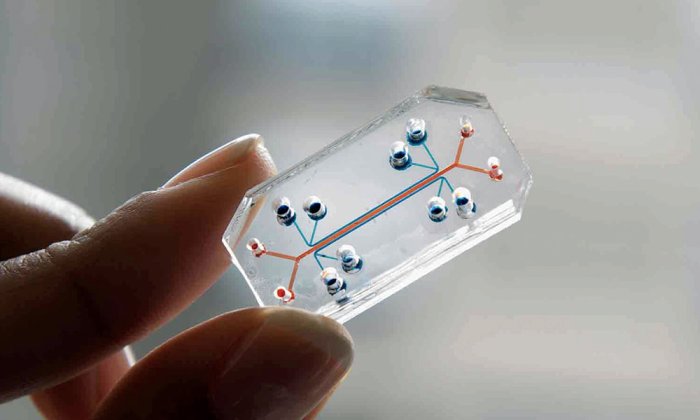
Organ-on-chip (OOC) technology has led to the development of multi-organ chip technology, which integrates multiple organ systems, such as the liver, kidney, and intestine, into a single platform to mimic the interactions that occur between organs in the human body. Replicating such complex physiological processes, multi-organ chips provide researchers the opportunity to study the pharmacokinetics and its overall systemic effects.
The metabolism using multi-organs chips as an emerging technology that is well suited to provide a species-specific platform to study the various types of metabolism including glucose, lipid, protein and drug metabolism by recreating organ-level function (2). In the recent past, researchers utilized a four-organ chip technology to study drug metabolism and toxicity. This chip replicated the interaction between different organs, enabling researchers to observe how a drug is absorbed, processed (metabolized), and eliminated.
MOCs enable researchers to model disease progression and drug interactions in a physiologically relevant environment, improving species translatability. To deliver high-resolution data for researchers that is easily analysed, enabling quick, personalized treatment for patients, OOCs are equipped with embedded sensors to measure pH, oxygen levels, and biochemical markers. The integration of MOC data within silico models enhances predictive power, aiding in personalized medicine and reducing reliance on animal testing.
To conclude, OOCs are transforming biomedical research with its enormous potential. This technology offers a more accurate, ethical, and cost-effective alternative to traditional methods, especially for drug testing, drug screening, drug response, and disease mechanisms. Furthermore, multi-organ chip technology holds much promise with changing paradigms of regulatory bodies (3), allowing the scientists to imitate the complex inter-organ interactions and predict the drug metabolism, toxicity, and systemic effects efficiently with an ethical approach to understanding and treating human diseases.
Reference
1. Biomedical Engineering and computational biology, “Lung-on-a-chip technology for disease modeling and drug development”, 2016
2. The Royal society, “Studying metabolism with multi-organ chips”, 2022
3. Cancers, “Organ-on-a-Chip and microfluidic platforms for oncology in the UK”, 2023
Image Credit: The MIT Press Reader